
Break The Chain
of Infection
Key Benefits
REDUCE RISK
Lower your risk of
cross-contamination with this
single-patient cuff solution.
Improve Financial
Outcomes
An affordable option to reduce costs associated with HAIs and those incurred with traditional cuff inventory and workflow.
ENHANCE PATIENT
SAFETY
A workflow where each patient gets a new disposable blood pressure cuff is a simple way to reduce risk associated with HAIs.

Research
“The high rate of BP cuff contamination (82.1%) observed in this study was not a surprise, as no other piece of hospital equipment was in more common use without adequate disinfection…”
A study in Singapore showed that most surfaces swabbed in an isolation room were contaminated, including the stethoscope. As a result, they concluded “Significant environmental contamination by patients with SAR-CoV-2 through respiratory droplets and fecal shedding suggests the environment as a potential medium of transmission and supports the need for strict adherence to environmental and hand hygiene.”
A hospital outbreak study carried out by scientists at the University of KwaZulu-Natal suggests all the cases originated from a single introduction, and that patients rarely infected other patients. Instead, the virus was mostly carried around the hospital by staff and on the surfaces of medical equipment. “We think in the main it’s likely to have been from [staff] hands and shared patient care items like thermometers, blood pressure cuffs, and stethoscopes,”
“Many different bacteria, viruses, fungi, and parasites may cause nosocomial infections… Clinicians and researchers should be aware of the risk of cross contamination of pathogens from inanimate surfaces in order to adopt appropriate infection control measures”.
“At the Japanese hospital… this investigation of contamination status using the gauze wiping method showed MRSA on 31.4% of blood pressure cuffs examined.”

Clinical Evidence

CDI: A COMMON CAUSE OF HAIs IN THE USA
Clostridium difficile infection (CDI) is recognized as the leading cause of gastroenteritis associated death and the most common cause of healthcare associated infections in the United States.
HAIs: A GROWING PROBLEM
WORLDWIDE
Hospital Acquired Infection or Healthcare Associated Infection (HAI) is a growing problem worldwide. On a given day, about 1 in 31 hospital patients has at least one healthcare-associated infection.


SARS-COV-2 AND HIGH TOUCHPOINTS
Two recent studies highlight the extent of SARS-CoV-2 environmental contamination and mode of transmission. Multiple surface sites were found to be contaminated including the bed rail, light switch, and stethoscope.
SINGLE PATIENT USE BP CUFFS: BREAK THE CHAIN OF INFECTION
Using disposable blood pressure cuffs may reduce the spread of infection and associated complications. This paper highlights the alarming amount of bacterial colonization on presumed clean cuffs. In one hospital setting, 100% of blood pressure cuffs cultured from the OR, PACU, BSICU, and ER contained bacterial colonization.


BP CUFFS: POTENTIAL VECTORS OF PATHOGENS
This collection of 8 clinical studies highlights the importance of recognizing BP cuffs as potential vectors of pathogenic bacteria among patients and as a source of reinfection.
BP CUFFS AND ASSOCIATED INFECTIONS
This collection of clinical study abstracts highlights the association of infection with the blood pressure cuff. One study showed that with the introduction of single-patient blood pressure cuffs there was an associated decrease in nosocomial infection rates.


NON-CRITICAL MEDICAL DEVICES AND HAI TRANSMISSION
This study assesses the role of non-critical medical devices, including thermometers and blood pressure cuffs in HAI transmission in a Nigerian teaching hospital. Results showed that 62.1% of thermometers and 82.1% of blood pressure cuffs examined were contaminated.
SPHYGMOMANOMETER CUFFS:
POTENTIAL SOURCE OF INFECTION
This study identifies sphygmomanometer cuffs as a potential source of infection. The microbiological investigations found 85% of cuffs were contaminated with bacterial organisms. Blood pressure cuffs are a frequently used tool in clinical practice.


BLOOD PRESSURE CUFFS: FRIEND OR FOE?
A study to assess the level of bacterial contamination of blood pressure cuffs in use on hospital wards was performed. Potential pathogens were isolated from 58% of cuffs, of which 33% had MSSA, 8% had MRSA and 33% had C. Diff.

Setting up an Isolation Room
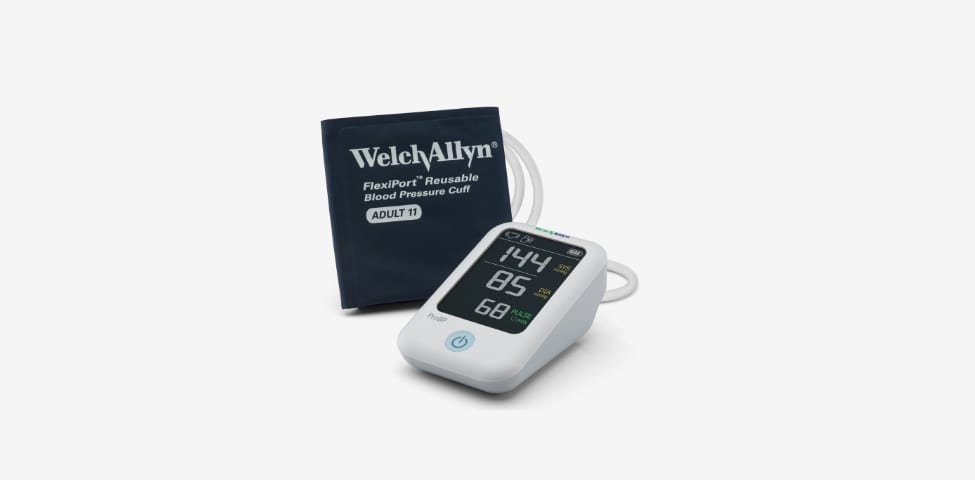
Recent studies have implicated the use of medical devices such as sphygmomanometers, thermometers, stethoscopes, and reusable blood pressure cuffs in the spread of HAIs. Hillrom can help.
Disposable and dedicated medical devices and equipment can reduce the risk of cross-contamination and are a proven method of successfully reducing HAIs. Hillrom offers a range of products providing your facility with an easy, cost-effective solution, from disposable blood pressure cuffs to blood pressure devices and ECG’s – which can help reduce the risk of cross-contamination, one patient at a time.
PRODUCT LIST
* Please note some products listed may not be available in your country.
Always Read Labels and Instructions for Use.




Infection Prevention Solutions
On any given day, about one in 31 hospital patients has at least one healthcare-associated infection.1 The Centers for Disease Control and Prevention (CDC) estimates hospital-acquired infections (HAIs) affect more than 1.7 million U.S. patients annually and cause about 99,000 deaths.2 The total cost to the healthcare system is estimated at $4.5 – $7.5 billion annually.3
A study in Singapore reported 11.9% patients with HAIs, primarily undetermined clinical sepsis, and pneumonia caused mainly by S. aureus and Pseudomonas aeruginosa. One systematic review and meta-analysis regarding HAIs in Southeast Asian countries (Brunei, Myanmar, Cambodia, East Timor, Indonesia, Laos, Malaysia, the Philippines, Singapore, Thailand, and Vietnam) found an overall prevalence rate of 9.1% with the most common microorganisms being P.aeruginosa, the Klebsiella species, and Acinetobacter baumannii.4
2. Klevens RM, Edwards JR, Richards CL, Horan TC. Estimating Health Care-Associated Infections and Deaths in U.S. 2002. Public Health Reports. 2007; 122: 160-166.
3. Stone PW, Larson E, Kawar LN. A systematic audit of economic evidence linking nosocomial infections and infection control interventions: 1990-2000. Am J Infect Control 2002; 30:145-52.
4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6245375/
PRODUCT LIST
* Please note some products listed may not be available in your country.
Always Read Labels and Instructions for Use.












































SINGAPORE
Hill-Rom Services Pte Ltd
1 Yishun Avenue 7
Singapore 768923
Phone +65 6499 7350
Fax +65 6499 7351
AUSTRALIA
Welch Allyn Australia Pty Ltd
Suite 4.01,2-4 Lyonpark Road
Macquarie Park NSW 2113
Australia
Phone 1800 445 576
CONNECT WITH US